After surviving a stay in the Intensive Care Unit (ICU), many patients face a long road to recovery. For individuals struggling with obesity, this journey can be particularly challenging. Recent research has shed light on the complex relationship between obesity and post-ICU health outcomes, highlighting the need for tailored support and intervention strategies.
A multicenter cohort study conducted in Brazilian ICUs compared the health-related quality of life (HRQoL) and functional status of patients across different body mass index (BMI) categories after three months post-ICU discharge. The study included 1600 ICU survivors, with outcomes assessed through structured telephone interviews and questionnaires.
Key Findings:
Lower Mental Component HRQoL: Obese patients reported lower scores in the mental component of HRQoL compared to normal-weight patients. This suggests that obesity may have a negative impact on psychological well-being during the recovery period.
No Significant Differences in Physical HRQoL or Functional Status: While differences were observed in the mental component of HRQoL, there were no significant distinctions among BMI categories regarding physical aspects of HRQoL or functional status. This indicates that obesity may not directly influence physical recovery after ICU discharge.
Lower Mortality Rates: Surprisingly, obese patients exhibited lower mortality rates compared to underweight and normal-weight patients. This phenomenon, known as the obesity paradox, challenges conventional assumptions about the relationship between obesity and mortality in critically ill patients.
Implications for Patient Care:
These findings have important implications for the care and management of post-ICU patients, particularly those struggling with obesity. Healthcare providers should:
Address Psychological Well-being: Recognize and address the psychological challenges faced by obese patients during the recovery process. Providing access to mental health support and counseling services can be beneficial in improving overall HRQoL.
Monitor Nutritional Status: While obesity may confer a survival advantage, it's essential to monitor nutritional status and address any deficiencies or malnutrition risk factors. A balanced diet and nutritional support can aid in optimal recovery and rehabilitation.
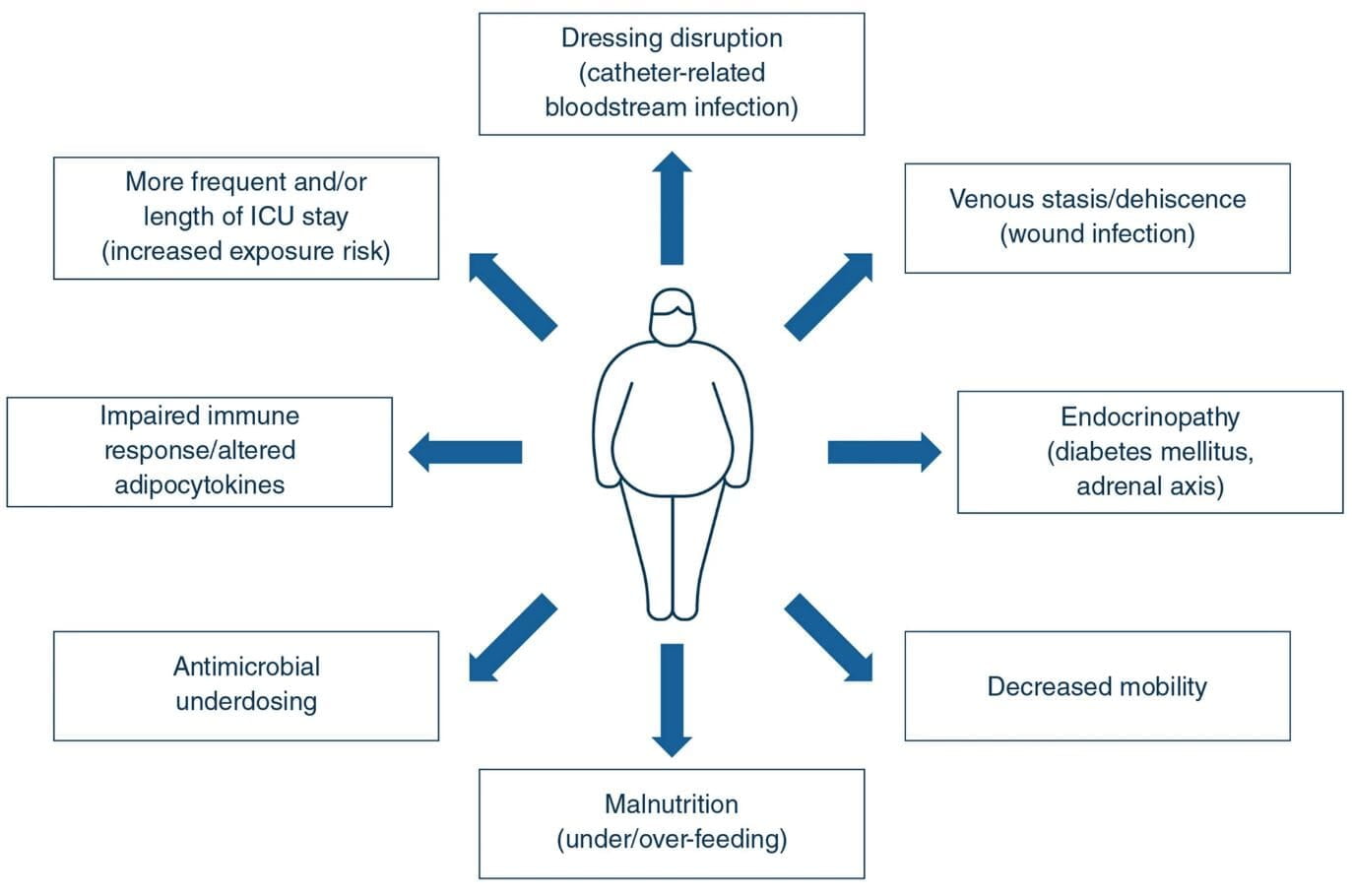
Individualized Care Plans: Recognize that one size does not fit all when it comes to post-ICU care. Develop individualized care plans that take into account the unique needs and challenges of obese patients, including mobility issues, medication dosages, and long-term lifestyle modifications.
Promote Physical Activity: Encourage gradual, appropriate physical activity as part of the recovery process. Physical rehabilitation programs tailored to obese individuals can help improve mobility, strength, and overall physical function.
Conclusion:
The study underscores the importance of considering obesity as a factor in post-ICU care and rehabilitation. By understanding the impact of obesity on health outcomes and implementing targeted interventions, healthcare providers can improve the quality of life and long-term prognosis for patients recovering from critical illness.
As patients of our obesity medicine clinic, it's essential to stay informed about the potential challenges and opportunities for recovery after an ICU stay. By working closely with our healthcare team and adopting proactive strategies for recovery, we can navigate the road to recovery with confidence and resilience.
